Abstract
The SARS-CoV-2 virus has infected hundreds of millions of people and caused millions of deaths worldwide. Reports of racial and ethnic disparities regarding both rates of infection of the SARS-CoV-2 virus and morbidity of the coronavirus disease-19 (COVID-19) contain profound differences depending on the population. A previous study found an independent and positive association between the Black/African American race and positive COVID-19 testing results in Milwaukee County, WI, while adjusting for age, sex, socioeconomic status, and comorbidities (Munoz-Price. et al, 2020, JAMA Network). Our previous study revealed that patients with COVID-19 who developed hypertriglyceridemia during their hospitalization were associated with a 2.3 times higher mortality rate, after adjusting for age, gender, body mass index, history of hypertension and diabetes (Dai. et al, 2021, manuscript accepted by Journal of Clinical Lipidology). Additionally, adverse blood clotting events is one of the major causes of death for patients with COVID-19. In this study, we investigated the correlation between racial/ethnic groups and mortality, along with potential correlations between hypertriglyceridemia and adverse blood clotting events in hospitalized patients with COVID-19 (ICD10CM:U07.1).
De-identified data from 1,441 hospitalized patients diagnosed with COVID-19 between March 2020 and June 2021 were extracted using the Medical College of Wisconsin Clinical Research Data Warehouse. Vital, demographic, and diagnostic information were used for the statistical analysis, specifically: age, gender, body mass index (BMI), race/ethnicity, thrombosis diagnosis and laboratory test results for triglyceride. The thrombotic events included were presence of disseminated intravascular coagulopathy, deep vein thrombosis, myocardial infarction, pulmonary embolism, and stroke diagnosed during their hospitalization. Hypertriglyceridemia was characterized as triglyceride levels greater than 150 mg/dL, with a baseline variable being the first occurrence of hypertriglyceridemia (baseline), and the peak variable being the highest manifestation of hypertriglyceridemia during hospitalization (peak).
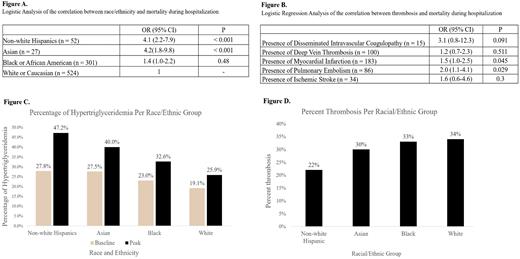
A binary logistic regression model showed that non-white Hispanic and Asian patients both had a higher correlation with mortality than white patients, with odds ratios (OR) of 4.1 [95% CI (2.2-7.9), p < 0.001] and 4.2 [95% CI (1.8-9.8), p < 0.001], respectively, after adjusting for age, BMI, and sex (Figure A). Additionally, the regression analysis showed that peak hypertriglyceridemia developed during hospitalization was correlated with a 1.8 times higher mortality in the entire inpatient cohort [95% CI (1.2-2.9), p < 0.01], after adjusting for age, sex, and BMI and independent of obesity. Furthermore, myocardial infarction [OR = 1.5, 95% CI (1.-2.5), p < 0.05] and pulmonary embolism [OR = 2.0, 95% CI (1.1-4.1), p < 0.05] were also correlated with a higher mortality, after adjusting for age, BMI, and sex (Figure B). The peak hypertriglyceridemia developed during hospitalization correlates with the incidence of thrombotic events with a borderline significance [OR= 1.5, 95% CI (0.9-2.1), p = 0.05] after adjusting for BMI, age, and sex. Further analysis revealed that non-white Hispanic patients had the highest frequencies of peak hypertriglyceridemia (triglyceride > 150 mg/dL) occurrence during hospitalization than the other race/ethnicity groups (Figure C). On the other hand, 22% of non-white Hispanics had at least one diagnosis of thrombotic event during hospitalization, which was the lowest incidence of thrombosis among all race/ethnicity groups (Figure D).
In our current retrospective study of inpatients with COVID-19, race/ethnicity, peak hypertriglyceridemia developed during hospitalization, and thrombosis are independently associated with mortality. The peak hypertriglyceridemia developed during hospitalization is positively correlated with the incidence of thrombosis.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal